Table of Contents
ToggleThroat infections can be a real nuisance, causing discomfort and disrupting daily life. When symptoms like pain and swelling arise, many people wonder if antibiotics are the right solution. Understanding when and how antibiotics can help is crucial for effective treatment and recovery.
Not all throat infections require antibiotics, especially since many are viral in nature. However, bacterial infections, such as strep throat, often necessitate antibiotic intervention. Knowing the signs of a bacterial infection and when to seek medical advice can make a significant difference in managing symptoms and preventing complications. This article will explore the role of antibiotics in treating throat infections, helping readers make informed decisions about their health.
Overview of Throat Infections
Throat infections can cause significant discomfort, affecting daily activities and quality of life. Two main types of throat infections exist: viral and bacterial. Viral infections, such as the common cold and influenza, often present with symptoms like a sore throat, cough, and runny nose. These infections usually resolve on their own without the need for antibiotics.
Bacterial infections, notably strep throat caused by Streptococcus bacteria, require antibiotic treatment. Strep throat typically showcases symptoms including severe sore throat, pain when swallowing, and fever. Recognizing these symptoms is crucial for determining whether medical attention is necessary.
Diagnostic methods, such as throat swabs and rapid strep tests, help distinguish between viral and bacterial infections. Health professionals often recommend seeking medical advice if symptoms persist for more than a few days or worsen. Early intervention plays a key role in preventing complications associated with untreated bacterial infections.
Understanding the type of infection is vital for effective treatment and recovery. Identifying patterns in symptoms leads to informed decisions regarding antibiotic use and overall throat health.
Common Causes of Throat Infections
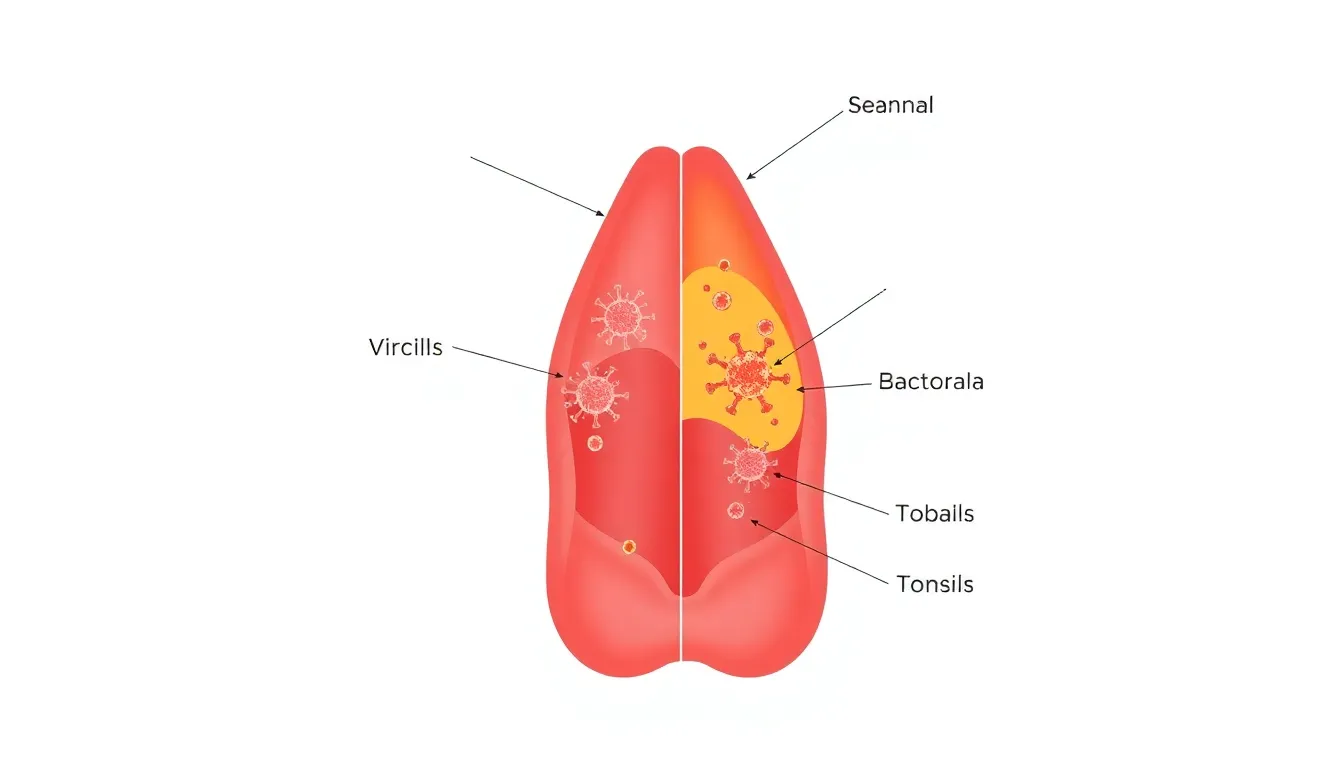

Throat infections can arise from various pathogens, primarily categorized into viral and bacterial origins. Recognizing the type of infection assists in determining the appropriate treatment approach.
Viral Infections
Viral infections account for the majority of throat infections. Common culprits include:
- Rhinovirus: Causes the common cold, presenting with sore throat, nasal congestion, and cough.
- Influenza virus: Symptoms include severe throat pain, fever, and body aches along with respiratory distress.
- Epstein-Barr virus: Associated with mononucleosis, it causes fatigue, swollen lymph nodes, and significant throat discomfort.
Most viral infections don’t require antibiotics, as symptoms typically resolve within a week, focusing instead on supportive care like hydration and rest.
Bacterial Infections
Bacterial infections, while less common, pose greater risks and often necessitate antibiotic treatment. Key examples include:
- Streptococcus pyogenes: Responsible for strep throat, characterized by intense sore throat, difficulty swallowing, swollen lymph nodes, and fever.
- Haemophilus influenzae: Can lead to epiglottitis or other respiratory complications, presenting with high fever and severe throat pain.
Bacterial infections often require rapid diagnostic tests or throat cultures to confirm the presence of bacteria, leading to timely and effective treatment to reduce risks of complications like rheumatic fever or kidney issues.
Understanding Antibiotics
Antibiotics play a crucial role in treating bacterial infections, including some throat infections like strep throat. Recognizing their purpose and mechanism can aid in appropriate use and understanding of their limitations.
What Are Antibiotics?
Antibiotics are medications designed to combat bacterial infections. They belong to various classes, such as penicillins, cephalosporins, and macrolides. Each class targets specific bacteria, making them effective for particular infections. However, antibiotics do not affect viral infections, highlighting the need for proper diagnosis before using these medications.
How Antibiotics Work Against Infections
Antibiotics work by disrupting essential processes within bacteria, ultimately inhibiting their growth or killing them. Common mechanisms include:
- Cell Wall Inhibition: Some antibiotics, like penicillin, prevent bacteria from forming a protective cell wall, leading to cell lysis.
- Protein Synthesis Inhibition: Others, such as tetracyclines, block bacterial ribosomes, disrupting protein production crucial for bacteria survival.
- DNA Replication Disruption: Fluoroquinolones alter DNA synthesis, halting bacterial replication.
These mechanisms effectively eliminate bacterial infections, relieving symptoms and preventing complications. Prompt treatment can significantly impact recovery, especially for severe infections.
Antibiotic Options for Throat Infections
Bacterial throat infections, such as strep throat, typically require antibiotic treatment. Selecting the appropriate antibiotic is crucial for effective management.
Common Antibiotics Prescribed
- Penicillin: Often the first choice for treating strep throat. It’s effective against Streptococcus pyogenes, the primary bacteria responsible for this infection. Patients usually complete a 10-day course for optimal results.
- Amoxicillin: Similar to penicillin but often preferred for its palatable taste. It also has a 10-day treatment regimen and provides adequate coverage against strep throat.
- Cephalosporins: Used if patients have a penicillin allergy. Medications like cephalexin are effective alternatives, targeting the same bacteria with a similar mechanism of action.
- Macrolides: Such as azithromycin or clarithromycin, serve as alternatives for those allergic to penicillin. These antibiotics work by inhibiting bacterial protein synthesis, offering a different treatment approach for strep throat.
Factors Influencing Antibiotic Choice
- Allergies: History of antibiotic allergies significantly impacts the selection process. Allergies to penicillin or related drugs necessitate alternative options like cephalosporins or macrolides.
- Bacterial Resistance: Local antibiotic resistance patterns influence prescribing habits. Physicians often consider these patterns to ensure effective treatment against prevalent bacterial strains.
- Patient Health History: Presence of chronic conditions or previous antibiotic use informs treatment decisions. It helps healthcare providers avoid prescribing antibiotics that may have less efficacy for the individual.
- Symptom Severity: Severe symptoms or complications increase the likelihood of aggressive treatment. In such cases, longer courses or stronger antibiotics may be necessary to ensure complete resolution of the infection.
Potential Side Effects of Antibiotics
Antibiotics can provide essential treatment for bacterial throat infections, but they may also lead to various side effects. Understanding these potential side effects ensures informed decision-making regarding antibiotic use.
- Gastrointestinal Issues
Antibiotics can disrupt the balance of bacteria in the gut, leading to nausea, diarrhea, or upset stomach. Symptoms vary between individuals, and some may experience more severe reactions, such as Clostridium difficile infection.
- Allergic Reactions
Allergic reactions to antibiotics can manifest as rashes, itching, or swelling. In more severe cases, anaphylaxis may occur, requiring immediate medical attention.
- Yeast Infections
Antibiotic use can sometimes promote yeast infections, especially in women. This occurs due to the destruction of beneficial bacteria, allowing yeast to overgrow.
- Photosensitivity
Certain antibiotics can increase sensitivity to sunlight, elevating the risk of sunburn or skin reactions when exposed to UV rays. Patients should take precautions, such as wearing sunscreen or protective clothing.
- Drug Interactions
Antibiotics may interact with other medications, altering their effectiveness. It’s crucial for patients to inform healthcare providers about all medications taken, including over-the-counter drugs and supplements.
- Long-term Effects
Prolonged antibiotic use can lead to resistance, making future infections more challenging to treat. This contributes to the growing concern of antibiotic resistance globally.
Awareness of these potential side effects aids healthcare providers and patients in making safer, informed decisions regarding antibiotic treatment for throat infections.







